读医学网
2010年欧洲帕金森综合征诊断和药物指南
发布时间:2014-05-19 10:34 类别:神经系统疾病 标签:initiated combinations gaps knowledge 来源:丁香园
Parkinson’s disease (PD) is a common neurodegenerative disorder with a cumulative effect on patients, their families and the healthcare and social care systems. In Scotland, there are between 120 and 230 patients with PD per 100,000 people. While the population of Scotland remains stable, the age related incidence of PD means that the number of cases will increase by 25–30% over the next 25 years.
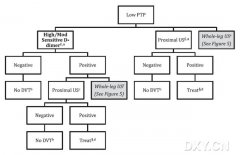
There are a wide range of drug treatments for Parkinson’s disease. However, it is not always clear which is the most appropriate treatment for the patient and whether the choice should be affected by age, clinical condition, or other factors. As the disease progresses, combination therapy is usually prescribed but there are gaps in clinical knowledge about when this should be initiated and what combinations of therapies are most effective.
Parkinson’s disease is a complex neurological disorder which can affect many aspects of the patient’s health and daily life. Ongoing ehabilitation in a patient with a progressive disease such as PD is best approached by a multidisciplinary team, which comprises several different professionals and services.
This guideline provides recommendations based on current evidence for best practice in the diagnosis and pharmacological management of PD. It includes comparisons of the accuracy of diagnoses carried out by different healthcare professionals, and the value of different diagnostic tests for differentiating PD from other associated conditions. It includes a comprehensive assessment of pharmacological management of motor and non-motor symptoms associated with PD. It also includes a narrative review of qualitative evidence describing the attitudes, beliefs and opinions of patients with PD across six themes. The role of the allied health professionals and the benefits of neurosurgical management of Parkinson’s disease, such as deep brain stimulation, have not been covered. The management of some non-motor symptoms is not included in this guideline as in many cases their management is not significantly different from that in people without Parkinson’s disease.
The management of patients with Parkinson’s disease covers a wide range of specialities, and this guideline will be of interest to general practitioners (GPs), neurologists, physicians, geriatricians, nurses working in hospitals, the community and care homes, pharmacists, psychologists, psychiatrists, patients, their carers and members of the voluntary sector. A wide range of medical disciplines is involved in routine management reflecting the fact that Parkinson’s disease is much more than simply a disorder of physical movement, and that the neurological involvement frequently causes symptoms across many different functional areas, such as mental health, bowel, bladder and blood pressure.